Get Back on Track with Practical ADHD Guidance
About this course
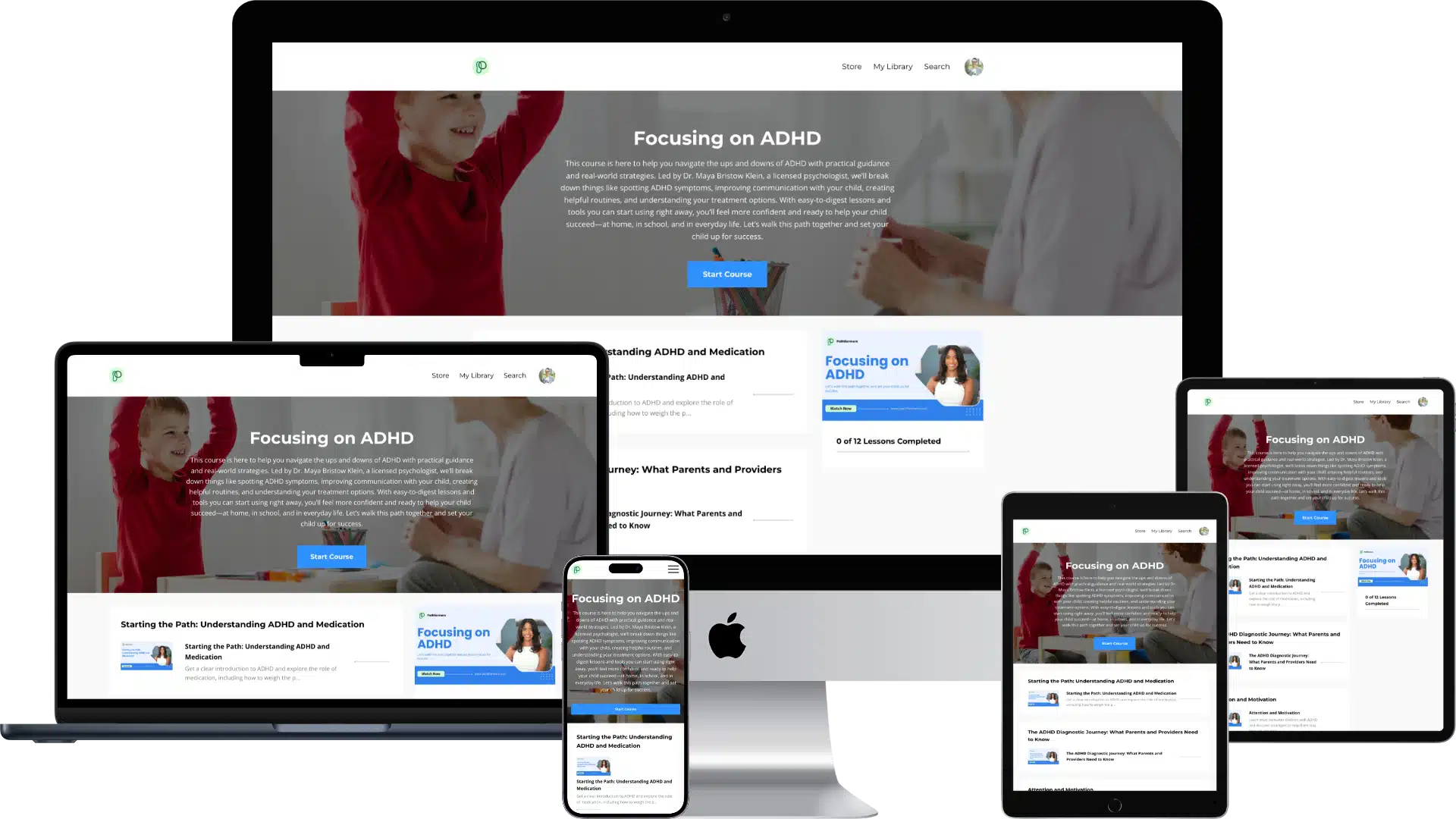
This course is here to help you navigate the ups and downs of ADHD with practical guidance and real-world strategies. Led by Dr. Maya Bristow Klein, a licensed psychologist, we’ll break down things like spotting ADHD symptoms, improving communication with your child, creating helpful routines, and understanding your treatment options. With easy-to-digest lessons and tools you can start using right away, you’ll feel more confident and ready to help your child succeed—at home, in school, and in everyday life. Let’s walk this path together and set your child up for success.
Overcoming ADHD Roadblocks One Step at a Time
Parenting a child with ADHD often feels like navigating an endless maze. You’ve likely spent countless hours researching, consulting experts, and trying different approaches, yet you still find yourself:
- Unsure of the right treatment path
- Struggling to effectively communicate with your child
- Frustrated by their ongoing focus issues
- Searching for real solutions that truly work
At Pathformers, we understand how overwhelming understanding and helping your child with ADHD can be. That’s why we developed “Focusing on ADHD”—an online course designed to cut through the confusion and provide the support you need when your child needs you the most.
Guided by Dr. Maya Bristow Klein, this course equips you with proven tools, actionable strategies, and expert support you need to help your child become the best version of themselves.

Your Path Forward
We’ve created this course to simplify ADHD and give you the clarity and confidence to move forward without feeling overwhelmed. It’s designed to help you better understand your child’s needs while offering real-world strategies that truly work.
Here’s what you can expect to learn:
Spotting the Signs of ADHD
Recognize the various ways ADHD shows up in kids and teens so you can take early action and make informed decisions.
Communicating Better with Your Child
Learn how to have more meaningful conversations that build trust and motivate your child in a way that works for them.
Building Structure at Home
Get practical tips to create a home environment that fosters focus and helps your child feel more in control of their day.
Exploring Medication and Alternatives
Gain balanced, straightforward guidance on medication options and alternatives, empowering you to make the right choice for your child.
Managing Emotional Ups and Downs
Understand the emotional side of ADHD and discover ways to help your child handle frustration, anxiety, and other common challenges.
Fostering Focus and Resilience
Learn how to boost your child’s ability to stay focused, manage distractions, and build resilience when faced with obstacles.
ADHD touches every aspect of your child’s life. This course equips you with the tools and support you need to help them feel understood, confident, and ready to thrive.
Parents Like You Trust Pathformers
What's Inside the Course
Each module is thoughtfully curated by Dr. Maya Bristow Klein, a licensed psychologist with years of experience working with children and teens. Dr. Klein breaks down the complexities of ADHD into clear, manageable steps, making it easier for you to understand and implement strategies. Along with engaging video lessons, you’ll have access to supporting worksheets, helpful resources, and actionable tools designed to help you apply what you learn every day.
Here’s a sneak peek at the course modules:
Starting the Path- Understanding ADHD and Medication
Get a clear introduction to ADHD and explore the role of medication, including how to weigh the pros and cons to make informed decisions for your child

The ADHD Diagnostic Journey: What Parents and Providers Need to Know
Learn how to get a proper ADHD assessment for your child. It covers why online tests aren’t reliable, what a full psychological evaluation involves, and how the results help you support your child effectively.
Attention and Motivation
Learn what motivates children with ADHD and discover strategies to help them stay focused and engaged in ways that work best for them.

Factors that Contribute to Attention
Understand the various factors, from environment to development, that influence your child’s ability to focus and how to set them up for success.

Supporting your Hyperactive Child Beyond Medication
Explore alternative approaches to managing hyperactivity without relying solely on medication, with actionable strategies for home and school.

Therapies and Support services for children with ADHD
Discover the different therapy options and support services available for children with ADHD, and how to choose the best fit for your family.
Building Focus and Resilience in Children with ADHD
Equip your child with tools to improve focus and develop resilience, helping them manage challenges with confidence and persistence.

Creating a structure home for children with ADHD
Learn how to create routines and structure at home that help your child feel more in control and ready to succeed.

Managing Emotional Challenges in Kids with ADHD
Understand the emotional struggles that often come with ADHD and learn strategies to help your child handle frustration, anxiety, and other feelings.

The influence of Trauma on ADHD
Explore how trauma can impact ADHD symptoms and learn how to address both challenges to better support your child’s emotional well-being.

Exploring Hidden Sadness in Children with ADHD
Recognize the signs of hidden sadness or frustration in children with ADHD and discover ways to help them express and process their emotions.
Exploring the Overlap between ADHD and Anxiety
Understand the link between ADHD and anxiety, and learn how to support your child in managing both conditions for better emotional and mental health.
Walking the Path Together
You don’t have to figure out ADHD on your own—we’re here to guide you. With expert tips, easy-to-use tools, and a down-to-earth approach, this course gives you everything you need to feel more confident and clear about what’s next.
Frequently Asked Questions
What does the “Focusing on ADHD” course cover?
It covers understanding ADHD, recognizing symptoms, improving communication, creating routines, and exploring treatment options like therapy and medication.
Is medication the only option for managing ADHD?
No, the course discusses medication along with therapy and relationship-based strategies for managing ADHD.
How can I help my child focus and manage ADHD at home?
You’ll learn tips for creating routines, boosting resilience, and enhancing focus using positive reinforcement and other methods.
How do I know if my child has ADHD?
The course helps parents identify key ADHD symptoms like attention difficulties, hyperactivity, and impulsivity.
What role does trauma play in ADHD?
The course explores the potential connection between early trauma and ADHD, helping parents understand how past experiences may influence their child’s behavior.
What Triggers Hyperactivity in ADHD?
Hyperactivity in children with ADHD often results from specific triggers. Recognizing these triggers can help parents and caregivers manage hyperactive behavior and create supportive environments. Common factors that trigger hyperactivity in ADHD include stress, poor sleep, overstimulation, and diet. Each of these elements plays a role in amplifying hyperactive tendencies, making it important to understand and mitigate their effects.
How Stress Triggers ADHD Hyperactivity
Stress is one of the main triggers of hyperactivity in children with ADHD. When children feel stressed, their brain’s ability to filter and process stimuli becomes even more impaired, leading to heightened hyperactivity. The connection between stress and hyperactivity lies in how the prefrontal cortex—the part of the brain responsible for focus and self-regulation—is affected. Research shows that stress can over-activate this region, increasing impulsive actions and hyperactive behavior.
Children with ADHD often feel overwhelmed by daily tasks like schoolwork, which adds to their stress. Parents can help by building routines that reduce stress, teaching relaxation techniques, and encouraging activities that provide a mental break, such as physical exercise and mindfulness practices.
The Impact of Poor Sleep on Hyperactivity
Sleep deprivation is another significant factor that can trigger ADHD hyperactivity. Lack of sleep worsens ADHD symptoms, including the ability to regulate movement and impulses. Inattention, forgetfulness, and increased restlessness all result from poor sleep, and children may show signs of hyperactivity as their brain struggles to stay alert. Ensuring children get at least 7 to 8 hours of sleep each night can help reduce these symptoms.
Does your child experience difficulty winding down at night? Many children with ADHD do, and this can lead to sleep deprivation, worsening their symptoms the next day. Parents can create bedtime routines that include winding down with calm activities, reducing screen time before bed, and ensuring the sleeping environment is free of distractions.
Overstimulation as a Trigger for Hyperactive Behavior
Overstimulation can overwhelm a child’s sensory system, leading to hyperactive behavior. Children with ADHD are particularly sensitive to sensory input, such as loud noises, bright lights, or crowded spaces. These stimuli make it harder for their brain to filter out excess information, resulting in increased movement and impulsivity.
For example, a noisy classroom or a bustling shopping mall can heighten hyperactivity. Parents can mitigate the effects of overstimulation by preparing their children for overwhelming situations. This might include providing coping tools such as earplugs, sunglasses, or teaching them to take sensory breaks in quieter environments.
Food and ADHD Hyperactivity
Certain foods and additives have been linked to increased hyperactivity in children with ADHD. Research suggests that sugary foods, simple carbohydrates, and food additives like sodium benzoate or MSG may exacerbate hyperactive behavior. On the other hand, foods rich in omega-3 fatty acids, proteins, and vitamins can help regulate ADHD symptoms.
If your child frequently experiences spikes in hyperactivity after meals, it may be worth keeping a food diary. Identifying specific foods that trigger hyperactivity allows for dietary adjustments that could lead to improvements in behavior.
The Role of Technology in ADHD Hyperactivity
The role of technology—particularly prolonged screen time—has been linked to hyperactive behavior in children with ADHD. Constant exposure to flashing images and rapid sensory input from electronic devices can overstimulate the brain. Studies have shown that more than two hours of screen time daily can significantly increase inattention and hyperactive behaviors.
Limiting screen time to structured segments and encouraging physical activity can help manage these triggers. Instead of lengthy screen sessions, engage your child in activities that help release energy, such as outdoor play or creative projects.
Managing ADHD Hyperactivity Triggers
Recognizing and managing hyperactivity triggers in children with ADHD can lead to significant improvements in their daily functioning. By reducing stress, ensuring proper sleep, minimizing overstimulation, and maintaining a balanced diet, you can create an environment that minimizes hyperactive tendencies. Managing these triggers isn’t always easy, but structured strategies and professional support can make a difference.
At our platform, we offer parents tools and expert advice to navigate the challenges of ADHD hyperactivity. By learning to identify and control these triggers, you can help your child achieve more balance in their day-to-day life.
Frequently Asked Questions (FAQs)
1. What triggers hyperactivity in ADHD?
Common triggers for hyperactivity in ADHD include stress, sleep deprivation, overstimulation, certain foods and additives, and excessive screen time. Each of these factors can amplify hyperactive behaviors in children.
2. How does stress affect hyperactivity in ADHD children?
Stress heightens hyperactivity by over-activating the prefrontal cortex, making it difficult for children to regulate their movements and impulses. Increased anxiety and pressure can lead to more pronounced hyperactive behaviors.
3. Can poor sleep trigger hyperactivity in children with ADHD?
Yes, sleep deprivation worsens ADHD symptoms, including hyperactivity. Children who don’t get enough sleep may show increased restlessness, impulsivity, and difficulty concentrating.
4. How can overstimulation trigger ADHD hyperactivity?
Overstimulation from loud noises, bright lights, or crowded environments overwhelms a child’s sensory system, often leading to increased hyperactivity as their brain struggles to filter excess stimuli.
5. Can food trigger hyperactivity in ADHD?
Yes, certain foods like sugary snacks, simple carbohydrates, and food additives may trigger hyperactivity. On the other hand, nutrients like omega-3 fatty acids and proteins can help reduce ADHD symptoms.
6. How does screen time affect hyperactivity in children with ADHD?
Prolonged screen time, especially over two hours a day, can overstimulate the brain, leading to increased inattention and hyperactivity. Limiting screen exposure and encouraging physical activity helps manage this trigger.
7. What strategies help manage ADHD hyperactivity triggers?
Strategies include reducing stress, ensuring adequate sleep, avoiding overstimulating environments, limiting screen time, and monitoring a child’s diet to avoid hyperactivity triggers.
What is Executive Dysfunction in Children with ADHD?
Q: What is executive dysfunction?
Executive dysfunction refers to difficulties with executive functions, which are mental skills crucial for planning, organizing, focusing, and managing time effectively. These skills help individuals set goals, remember instructions, and handle multiple tasks simultaneously.
Q: How does executive dysfunction relate to ADHD?
Children with ADHD often experience executive dysfunction due to differences in brain activity that affect self-control and goal-directed behavior. This makes it challenging for them to perform tasks that require planning, organization, and focused attention.
Q: What are the common signs of executive dysfunction in children with ADHD?
Some of the common signs include:
- Impulse Control: Difficulty restraining impulses, leading to behaviors like interrupting others or acting without thinking.
- Time Management: Struggles with perceiving time, estimating how long tasks will take, or transitioning between activities.
- Working Memory: Problems holding information in mind to complete tasks, affecting their ability to follow multi-step instructions.
- Flexibility: Difficulty adapting to changes or switching strategies, making them appear rigid or inflexible.
- Organization: Challenges organizing tasks and materials, which can lead to messy workspaces and difficulty managing homework.
- Planning and Prioritization: Trouble setting up plans, determining task sequences, and identifying which tasks are most important.
- Self-Monitoring: Difficulty assessing their own performance, which affects learning from past experiences.
- Emotion Regulation: Struggles with managing emotions, leading to issues with frustration, excitement, or disappointment.
Q: How can executive dysfunction impact a child’s daily life?
Executive dysfunction can affect academic performance, social interactions, and daily activities. For example, a child might find it difficult to complete homework on time, struggle with following rules during group activities, or become easily frustrated when things don’t go as planned.
Q: Can children with ADHD overcome executive dysfunction?
Yes, with appropriate strategies and interventions, children can learn to manage or reduce the challenges of executive dysfunction. Techniques like behavioral therapy, organizational coaching, and sometimes medication can help improve executive skills, allowing children to develop better coping mechanisms and more effective ways of handling tasks.
Q: What types of strategies can help children with executive dysfunction?
- Routine Building: Establishing consistent daily routines can help children manage time and tasks more effectively.
- Visual Aids and Checklists: Tools like calendars, planners, and to-do lists can support organization and planning.
- Break Tasks into Steps: Simplifying tasks into smaller, manageable parts makes them easier to complete.
- Teach Time Management Skills: Using timers and alarms can help children understand time and stay on track.
- Positive Reinforcement: Encouraging and rewarding small successes can motivate children to build executive skills gradually.
Understanding and supporting children with executive dysfunction is key to helping them navigate the challenges associated with ADHD. With the right support, they can develop skills to improve their academic, social, and everyday lives.
How to Calm Down an ADHD Child?
1. Why do children with ADHD often struggle to calm down?
Children with ADHD frequently experience difficulty regulating their emotions due to heightened impulsivity and hyperactivity. These challenges, combined with an inability to focus or effectively express frustration, can lead to emotional outbursts or feelings of being overwhelmed. Understanding these reactions is key to providing the right support.
2. What are effective ways to help an ADHD child regain composure?
Several strategies can help a child with ADHD calm down:
- Practice Relaxation Techniques: Teach deep breathing, mindfulness, or progressive muscle relaxation to help manage stress and anxiety.
- Consistent Parenting: Establish clear, predictable rules and consequences to create a sense of security.
- Break Up Tasks: Divide homework or chores into manageable segments with short breaks for physical activity.
- Provide Fidget Tools: Offer stress balls or sensory toys to help release energy in a constructive way.
- Encourage Play Before Big Tasks: Allow active play before homework or household responsibilities to improve focus.
3. How can fidgeting be redirected positively?
Fidgeting is a natural way for children with ADHD to manage their energy and focus. Rather than discouraging it, provide tools like:
- Stress balls
- Sensory toys
- Fidget spinners or cubes
These tools help channel restlessness constructively, improving concentration in school or social settings.
4. Why is play important for children with ADHD?
Play provides a healthy outlet for energy, stress relief, and social skill development. Activities like sports, dance, or creative play allow children to:
- Express themselves.
- Practice problem-solving.
- Prepare for focus-driven tasks.
Encouraging active play before homework or other challenging activities can reduce frustration and improve task engagement.
5. What role do relaxation techniques play in calming ADHD symptoms?
Relaxation techniques, such as:
- Deep Breathing: Helps slow the heart rate and reduce anxiety.
- Progressive Muscle Relaxation: Relieves tension through step-by-step relaxation of muscle groups.
- Mindfulness: Enhances self-awareness and emotional control.
These techniques empower children to self-regulate, manage overwhelming emotions, and build confidence.
6. How can parents create a calming environment for an ADHD child?
A structured, predictable routine helps children feel secure and less overwhelmed. Strategies include:
- Organizing the Day: Use visual schedules or to-do lists to prioritize tasks.
- Breaking Tasks into Steps: Divide activities into smaller, manageable parts.
- Minimizing Distractions: Create a quiet, organized space for homework and relaxation.
A calm, structured environment reduces stress and enhances productivity for children with ADHD.
7. How can parents stay calm during challenging moments?
Parenting a child with ADHD can be demanding, but self-care is vital. Parents can:
- Practice mindfulness or relaxation techniques.
- Maintain regular exercise and healthy routines.
- Share caregiving responsibilities with a partner or trusted individual.
- Seek support from ADHD-focused resources or professional guidance.
8. How can Pathformers help parents and caregivers?
Pathformers offers evidence-based resources and strategies tailored to the unique challenges of raising a child with ADHD. Through research-backed courses and practical tools, Pathformers empowers families to:
- Create structured, supportive environments.
- Foster emotional regulation and resilience.
- Implement actionable strategies for managing ADHD symptoms effectively.
Take the Next Step with Pathformers
Empower your family with the tools and techniques needed to support your child with ADHD. Explore Pathformers’ expert-designed courses and resources to create a calm, structured, and nurturing environment for positive growth. Explore our courses today!
Can ADHD Cause Emotional Dysregulation?
1. What is emotional dysregulation in ADHD?
Emotional dysregulation is a common challenge for individuals with ADHD, characterized by difficulty managing emotional responses. This can lead to intense feelings that may arise quickly, linger, or feel overwhelming. Emotional dysregulation often shows up as irritability, impulsive reactions, or heightened sensitivity to criticism or perceived rejection, making everyday interactions more complex.
2. Is emotional dysregulation a recognized part of ADHD?
Yes, emotional dysregulation is increasingly recognized as a fundamental aspect of ADHD, although it is currently listed as an “associated feature” in diagnostic guidelines. Researchers and clinicians are now acknowledging its significant impact on individuals with ADHD. This feature is seen across all ADHD subtypes, with those diagnosed with the combined subtype typically showing the highest levels of emotional dysregulation.
3. How does ADHD affect emotional responses?
ADHD impacts both “bottom-up” emotional reactivity (how quickly and intensely emotions arise) and “top-down” regulatory control (the ability to manage and moderate these emotions). This combination can make individuals with ADHD more prone to emotional outbursts, heightened frustration, and prolonged reactions to stressors. Pathformers provides insights into managing these responses, helping parents and children develop effective strategies to support emotional well-being.
4. Why is emotional dysregulation in ADHD sometimes overlooked?
Emotional dysregulation has historically been overshadowed by the core ADHD symptoms of inattention, hyperactivity, and impulsivity. Many clinicians may be more familiar with diagnosing mood disorders, like depression or anxiety, in cases of emotional challenges, which can sometimes lead to a delay in recognizing ADHD’s role. However, as awareness grows, more clinicians are incorporating emotional aspects into their ADHD evaluations, supporting a more comprehensive understanding of the condition.
5. Can emotional dysregulation impact social relationships?
Yes, emotional dysregulation can have a significant effect on social interactions. Intense emotions may lead to impulsive reactions, difficulty managing criticism, or a tendency to withdraw. These challenges can influence friendship quality, family dynamics, and relationships at school or work. Recognizing and addressing these emotional challenges early on can help improve social interactions and build healthier connections.
6. How does emotional dysregulation affect children differently from adults?
In children with ADHD, emotional dysregulation can manifest as sudden anger, frustration, or exaggerated reactions to minor setbacks. Children may also struggle to identify and name their emotions, leading to misunderstandings or prolonged distress. For adults, emotional dysregulation often correlates with the severity of ADHD symptoms, making work and personal relationships more challenging. Pathformers provides resources to help parents understand and navigate these age-specific emotional challenges.
7. What strategies help manage emotional dysregulation in ADHD?
Behavioral approaches like cognitive behavioral therapy (CBT), social skills training, and structured routines are valuable in managing emotional dysregulation. These methods teach individuals with ADHD to recognize their emotions, consider the consequences of impulsive reactions, and reframe situations constructively. Pathformers emphasizes these strategies in our courses, offering practical tools for families to use in daily life.
8. Can medication help with emotional dysregulation in ADHD?
While stimulant medications are often prescribed to manage inattention and hyperactivity in ADHD, their effect on emotional dysregulation varies. Some medications, like methylphenidate, have shown promise in reducing emotional symptoms in children and adults with ADHD, though results may differ. Behavioral interventions remain a key component, as they address both emotional regulation and the skills needed for managing everyday interactions.
9. Is rejection sensitivity related to ADHD?
Yes, many individuals with ADHD experience heightened sensitivity to rejection or criticism, a phenomenon known as rejection-sensitive dysphoria. This sensitivity can lead to intense emotional reactions when perceived rejection occurs. Pathformers’ resources provide guidance on coping with rejection sensitivity, helping individuals develop resilience and improve their social interactions.
10. How can parents support a child with ADHD and emotional dysregulation?
Parents play a central role in helping children manage emotional dysregulation. By creating a structured, supportive environment and using positive reinforcement, parents can guide children in recognizing and responding to their emotions. Pathformers offers practical resources and training to empower parents with strategies that make a meaningful difference in their child’s emotional and social development.
Does ADHD Cause Poor Working Memory?
1. What is working memory, and how is it related to ADHD?
Working memory is a crucial component of executive function, allowing individuals to hold and manipulate information in real-time. For children with ADHD, working memory deficits often make it difficult to remember and execute tasks, leading to challenges in academics, social interactions, and daily routines.
2. How does ADHD affect working memory?
ADHD disrupts the brain’s executive function, including working memory. The ADHD brain often struggles to store short-term memory effectively, causing difficulties with:
- Remembering multi-step instructions.
- Retaining details long enough to use them.
- Organizing information in tasks like writing or math.
3. What are the symptoms of working memory deficits in ADHD?
Children with ADHD and poor working memory may exhibit:
- Difficulty following through on instructions.
- Frequently forgetting daily tasks like homework or chores.
- Trouble staying focused during multi-step activities.
- Struggles with recalling details in conversations or lessons.
4. Is working memory the same as short-term memory?
While related, working memory is more complex than short-term memory. It not only involves holding information temporarily but also using it actively, such as solving a math problem or following a recipe. In ADHD, both working memory and short-term memory can be impaired.
5. How do working memory deficits impact learning in children with ADHD?
Poor working memory can significantly hinder academic success. For example:
- Math: Difficulty recalling numbers or steps in multi-step problems.
- Reading: Losing track of context while processing sentences or paragraphs.
- Writing: Forgetting ideas or struggling to organize sentences cohesively.
6. Can poor working memory in ADHD lead to memory loss?
While ADHD does not cause true memory loss, working memory deficits can feel like forgetfulness or memory gaps. Children with ADHD may struggle to recall information they recently learned or were just told, leading to repeated mistakes or misunderstandings.
7. Are there strategies to support working memory in children with ADHD?
Yes, parents and educators can implement several techniques to help children with ADHD:
- Use visual aids like charts, checklists, and reminders.
- Break tasks into smaller steps to reduce memory load.
- Encourage repetition and rehearsal to reinforce new information.
- Establish consistent routines to minimize reliance on memory.
- Use tools like timers or alarms for reminders.
8. Can working memory improve in children with ADHD?
Yes, with targeted interventions and consistent practice, children with ADHD can develop strategies to manage their working memory challenges. Activities like memory games, mindfulness exercises, and structured learning support can help strengthen these skills.
9. How does Pathformers help families address working memory deficits in ADHD?
Pathformers provides evidence-based courses and resources tailored to support executive function development, including working memory. These programs empower parents and educators with actionable strategies to improve focus, organization, and memory in children with ADHD.
10. What should parents do if working memory deficits significantly impact their child’s life?
If working memory deficits interfere with daily functioning or learning, parents should seek guidance from professionals like educational psychologists or ADHD specialists. Early intervention can lead to better outcomes and a more structured support plan for the child.
What Are the Comorbidities of Childhood Depression?
Childhood depression, also known as depressive disorders in children and adolescents, often coexists with other mental health conditions. These comorbidities can intensify challenges and necessitate an integrated approach for effective management. Below, we explore the most common comorbidities, their implications, and strategies for support.
What Is Comorbidity in Childhood Depression?
Comorbidity refers to the presence of one or more additional disorders alongside depression in children and adolescents. This coexistence complicates diagnosis and treatment, impacting the mental health and overall well-being of the affected individual.
What Are the Most Common Comorbidities of Childhood Depression?
1. Anxiety Disorders
- Overview: Includes generalized anxiety disorder, social anxiety, and panic disorder.
- Prevalence: Many children with depression also exhibit symptoms of anxiety, creating a complex clinical picture.
- Impact: Heightened emotional distress, impaired functioning, and challenges in school and social settings.
2. Attention-Deficit/Hyperactivity Disorder (ADHD)
- Overview: Symptoms of hyperactivity, impulsivity, and inattention often overlap with depression.
- Prevalence: Studies estimate that 13% to 27% of children with ADHD also experience depression.
- Impact: Requires tailored treatment strategies to address both conditions effectively.
3. Conduct Disorder
- Overview: Characterized by aggressive or antisocial behaviors.
- Impact: Coexisting conduct disorder can exacerbate behavioral issues, increasing academic and social difficulties.
4. Substance Use Disorders
- Overview: Adolescents with depression are at higher risk for substance use disorders.
- Impact: Substance use worsens depressive symptoms and hinders recovery.
5. Learning Disabilities
- Overview: Conditions like dyslexia often coexist with depression.
- Impact: Struggles in school contribute to low self-esteem, exacerbating depressive symptoms.
What Are the Risk Factors for Comorbidity in Childhood Depression?
Common risk factors include:
- Family History: A genetic predisposition to depression or anxiety.
- Stressful Life Events: Trauma, abuse, or significant life changes.
- Developmental Challenges: Cognitive, emotional, or social difficulties that increase vulnerability.
How Does Comorbidity Affect the Treatment of Childhood Depression?
Comorbidities often require:
- Integrated Approach: Simultaneously addressing depression and co-occurring disorders.
- Therapeutic Strategies: Adapting interventions like cognitive-behavioral therapy (CBT) to manage overlapping symptoms.
- Monitoring and Adjustment: Regular evaluations to assess progress and modify treatment plans as needed.
How Can Parents and Caregivers Support Children with Comorbid Depression?
Parents and caregivers play a vital role in supporting children with depression and comorbid conditions. Key steps include:
- Seek Professional Help: Work with mental health specialists trained in child and adolescent care.
- Encourage Open Communication: Foster a safe, non-judgmental environment for children to share their feelings.
- Promote Healthy Habits: Ensure routines include sufficient sleep, regular exercise, and a balanced diet.
- Stay Informed: Learn about your child’s specific comorbidities to better understand and meet their needs.
What Are the Next Steps for Managing Comorbidities in Childhood Depression?
- Early Diagnosis: Timely identification improves outcomes.
- Comprehensive Treatment Plans: Collaborate with professionals to tailor strategies to your child’s unique needs.
- Consistent Support: Maintain a supportive home environment and prioritize regular check-ins with healthcare providers.
For more resources and expert guidance on managing childhood depression and its comorbidities, explore Pathformers’ educational materials and advocacy programs. Together, we can provide the support children need to thrive.
What Neurological Deficits Occur in ADHD?
1. Is ADHD a neurological condition?
Yes, ADHD is a neurological condition affecting how the brain processes information. It involves differences in brain structure, function, and connectivity, influencing attention, impulse control, and emotional regulation. These differences help explain many challenges faced by individuals with ADHD.
2. What areas of the brain are affected by ADHD?
ADHD is associated with differences in several key brain regions:
- Prefrontal Cortex: Manages executive functions like decision-making, attention, and impulse control.
- Basal Ganglia: Involved in motor control and emotional regulation.
- Cerebellum: Coordinates timing and attention.
- Limbic System: Influences emotional processing and motivation.
These areas work together to manage focus, behavior, and emotions. Differences in these regions contribute to ADHD symptoms.
3. How does ADHD affect brain chemistry?
ADHD is linked to imbalances in neurotransmitters, particularly dopamine and norepinephrine:
- Dopamine: Regulates reward and motivation.
- Norepinephrine: Influences focus and attention.
Imbalances can lead to difficulties in sustaining attention, controlling impulses, and managing emotions.
4. Are brain structures different in individuals with ADHD?
Yes, studies reveal slight differences in brain size and activity for individuals with ADHD. For example, the prefrontal cortex may be smaller or less active, affecting executive functions like planning, self-regulation, and decision-making.
5. How do these neurological deficits impact daily functioning?
Neurological deficits in ADHD can affect:
- Focus: Difficulty maintaining attention on tasks.
- Organization: Struggles with planning and time management.
- Emotional Regulation: Increased frustration or impulsivity.
- Task Completion: Challenges with activities requiring sustained mental effort.
Understanding these factors is essential for developing effective interventions.
6. Can neurological deficits in ADHD change over time?
Yes, brain development and neuroplasticity mean that some aspects of ADHD may change with age. For example:
- Hyperactivity: Often decreases in adolescence.
- Inattention and Executive Function Challenges: May persist into adulthood.
Early intervention can help individuals adapt and develop coping strategies.
7. Are these neurological differences genetic?
There is some research suggesting that ADHD has a strong genetic component. Inherited traits influence brain structure and function, while environmental factors, such as prenatal exposure to stress or toxins, can also contribute to neurological differences.
8. How can understanding ADHD’s neurological basis help in managing the condition?
Recognizing ADHD as a neurological condition highlights the need for evidence-based strategies, such as:
- Behavioral Therapy: Helps manage emotional regulation and behavior.
- Pharmacological Intervention: Addresses neurotransmitter imbalances.
- Structured Routines: Supports executive function development.
These approaches target the root causes of ADHD symptoms, helping individuals thrive.
9. What role does neuroplasticity play in ADHD?
Neuroplasticity is the brain’s ability to adapt and form new connections over time. With interventions like:
- Skill-Building Exercises
- Therapy
- Mindfulness Training
Individuals with ADHD can develop alternative pathways to manage challenges and improve functioning.
10. How does Pathformers support families in understanding these neurological aspects?
Pathformers provides evidence-based resources and courses tailored to the neurological aspects of ADHD. Our programs focus on:
- Attention Support: Practical tools to enhance focus.
- Emotional Regulation: Strategies to build resilience.
- Executive Functioning: Skills for managing tasks and time.
Explore our offerings to empower your family with the knowledge and tools to support children with ADHD.
Take the Next Step with Pathformers
Pathformers is dedicated to helping families understand and address the neurological aspects of ADHD. Start your journey today with our expert-designed resources and courses, providing actionable strategies for a brighter future. Discover how you can make a difference! Explore our courses today!
How Does ADHD Affect Psychological Development?
1. What is the impact of ADHD on psychological development?
ADHD affects psychological development by challenging a child’s ability to focus, regulate emotions, and build social relationships. These difficulties can delay emotional and social maturity, and may persist into adulthood if untreated. Co-occurring conditions, such as anxiety, depression, or learning disabilities, often compound these challenges, making psychological development more complex.
2. How does ADHD manifest differently in childhood and adolescence?
- Childhood: Symptoms such as inattention, hyperactivity, and impulsivity are prominent. These can disrupt learning, peer interactions, and family relationships.
- Adolescence: Hyperactivity often decreases, but inattention and impulsivity remain. Emotional regulation challenges may become more internalized, leading to heightened sensitivity to rejection, academic struggles, and risk-taking behaviors.
3. What are comorbid conditions, and how do they affect individuals with ADHD?
Comorbid conditions—such as anxiety, depression, learning disabilities, or conduct disorders—frequently coexist with ADHD. They can intensify emotional and cognitive challenges, complicate diagnosis, and hinder treatment. For instance:
- ADHD + Anxiety: May lead to heightened emotional reactivity.
- ADHD + Learning Disabilities: Amplifies academic struggles, potentially lowering self-esteem.
4. How does ADHD impact social and emotional development?
ADHD often impairs the ability to interpret social cues, regulate emotions, and control impulses, leading to challenges such as:
- Difficulty forming and maintaining friendships.
- Increased peer rejection or conflicts.
- A feedback loop of negative social interactions, which can worsen emotional well-being.
- Early intervention can help mitigate these issues and build stronger social skills.
5. Can untreated ADHD lead to long-term psychological issues?
Yes, untreated ADHD can contribute to:
- Chronic low self-esteem.
- Increased risk of substance use disorders.
- Development of mood disorders or antisocial behaviors.
- Timely diagnosis and treatment are essential for preventing these outcomes and supporting healthy development.
6. How do gender differences influence the psychological development of individuals with ADHD?
- Boys: Often display externalized symptoms (e.g., hyperactivity, impulsivity), leading to earlier recognition.
- Girls: More likely to exhibit internalized symptoms (e.g., inattention, emotional dysregulation), often misdiagnosed as anxiety or depression.
- These differences emphasize the need for tailored diagnostic and treatment approaches.
7. What role do sleep disorders play in the psychological development of children with ADHD?
Sleep disorders, such as insomnia or sleep apnea, are common in ADHD and exacerbate symptoms like:
- Inattention and hyperactivity.
- Emotional dysregulation and irritability.
- Addressing sleep issues alongside ADHD treatment can enhance cognitive functioning and improve overall quality of life.
8. How can early intervention improve psychological outcomes for individuals with ADHD?
Early intervention supports psychological development by:
- Addressing core symptoms to reduce academic and social challenges.
- Managing comorbid conditions to alleviate additional stress.
- Teaching coping mechanisms and emotional regulation strategies to foster resilience and self-confidence.
9. What strategies support the psychological development of children and adolescents with ADHD?
- Structured Environments: Consistent routines provide stability.
- Positive Reinforcement: Rewards for desired behaviors encourage skill-building.
- Self-Regulation Techniques: Teach mindfulness and emotional awareness.
- Parent Training: Helps families implement effective strategies for managing ADHD symptoms.
Pathformers offers evidence-based resources for parents and caregivers to support these strategies.
10. Why is it important to address comorbid conditions alongside ADHD treatment?
Comorbid conditions can intensify ADHD-related challenges, such as:
- Amplifying emotional or academic struggles.
- Complicating the development of coping mechanisms.
- A comprehensive treatment plan that includes managing comorbid conditions ensures a more holistic approach, fostering improved outcomes in psychological development.
Supporting psychological development in individuals with ADHD requires a multi-faceted approach. Early intervention, addressing comorbidities, and implementing targeted strategies are key to helping children and adolescents thrive.
For more resources and support, explore Pathformers’ evidence-based courses and tools for families and caregivers.
Does ADHD Cause Trouble Sleeping?
1. Can ADHD affect sleep patterns?
Yes, ADHD is often associated with sleep challenges. Individuals with ADHD may experience difficulty falling asleep, staying asleep, or waking up in the morning. These issues can stem from heightened mental activity, difficulty winding down, or coexisting conditions that disrupt sleep.
2. What types of sleep issues are common in people with ADHD?
Common sleep challenges for individuals with ADHD include:
- Insomnia: Trouble falling asleep or staying asleep.
- Restless Sleep: Frequent movement or waking during the night.
- Delayed Sleep Phase Syndrome (DSPS): A shifted sleep schedule where falling asleep and waking up occur later than usual.
- Restless Legs Syndrome (RLS): An uncontrollable urge to move the legs, especially at night.
- Sleep Apnea: Interrupted breathing during sleep, leading to fatigue and restlessness.
3. Why does ADHD cause sleep problems?
ADHD-related sleep difficulties may arise due to:
- Neurological Differences: ADHD affects the brain’s regulation of arousal and relaxation, making it harder to transition into sleep.
- Hyperactivity and Impulsivity: These symptoms can keep individuals physically or mentally restless, delaying the onset of sleep.
- Emotional Dysregulation: Anxiety, frustration, or overstimulation can interfere with a calm bedtime routine.
4. How do sleep problems impact ADHD symptoms?
Sleep issues can worsen ADHD symptoms such as inattention, hyperactivity, and mood swings. Poor sleep reduces the brain’s ability to focus, regulate emotions, and process information, creating a cycle where ADHD symptoms and sleep challenges feed into each other.
5. Are children with ADHD more likely to have sleep issues than adults?
While both children and adults with ADHD can experience sleep challenges, the nature of these issues may vary:
- Children: Struggle with bedtime resistance and restlessness.
- Adults: May face insomnia, delayed sleep schedules, or fatigue that affects daily functioning.
6. What strategies can help manage sleep problems in individuals with ADHD?
Several approaches can support better sleep for individuals with ADHD:
- Establish a Consistent Routine: Set regular sleep and wake times to regulate the body’s internal clock.
- Create a Calm Environment: Reduce noise, light, and distractions in the bedroom.
- Limit Stimulants: Avoid caffeine and electronic screens before bedtime.
- Practice Relaxation Techniques: Activities like deep breathing, meditation, or reading can help signal the body to wind down.
- Consult a Specialist: Healthcare providers can offer tailored recommendations or address underlying conditions like sleep apnea or RLS.
7. Can medication for ADHD affect sleep?
Yes, some stimulant medications used to treat ADHD can interfere with sleep, especially if taken late in the day. Non-stimulant medications or adjustments to dosing schedules may help minimize these effects. Always consult with a healthcare provider about medication concerns.
8. Are there behavioral approaches to improve sleep in ADHD?
Behavioral strategies, such as cognitive behavioral therapy for insomnia (CBT-I), have shown promise in improving sleep for individuals with ADHD. These techniques address habits and thought patterns that interfere with sleep, promoting healthier routines and restful nights.
9. How can parents support a child with ADHD who struggles to sleep?
Parents can support their child’s sleep by:
- Creating a calming bedtime routine with activities like reading or quiet play.
- Ensuring the child’s bedroom is free from distractions.
- Encouraging consistent sleep schedules, even on weekends.
- Consulting a pediatrician for guidance on managing sleep challenges specific to ADHD.
10. How does Pathformers support families dealing with ADHD and sleep challenges?
Pathformers provides evidence-based courses and resources that empower families to address ADHD-related challenges, including sleep difficulties. By equipping parents with actionable strategies, Pathformers helps improve both sleep and daily functioning, creating a foundation for growth and well-being.
Find Solutions for Better Sleep with Pathformers
Explore our ADHD-focused resources to learn effective strategies for managing sleep challenges and empowering your family to thrive. Explore our courses today for expert guidance and actionable tools.
Help Steer Your Child’s Development
Subscribe to our newsletter for exclusive video updates, expert parenting strategies, and the latest insights in child development and mental health.




